Scent is a powerful time portal, reviving long-forgotten memories in stark detail. The human brain begins to build a library of smells in infancy, which grows into adulthood. For people with hereditary hyperosmia—a rare, heightened ability to detect and discern scents—this smell repository can be vast and remarkably fine-tuned. Joy Milne, a retired nurse, patient advocate, researcher, and grandmother, discovered this superpower as a child.1 Milne’s grandmother—also a super sniffer—trained her to identify scent signatures, as her own mother had taught her. As a nurse, Milne acquired an extensive clinical scent library, recognizing patterns between disease symptoms and diagnoses. After her late husband’s Parkinson’s disease (PD) diagnosis, she realized that the musky smell he wore at the nape of his neck for over a decade was an early warning sign and that she could detect it in other PD patients.
See “Chemicals on the Skin Could Enable Parkinson’s Detection”
Milne is now on a mission to fulfill the promise she made on her husband’s deathbed to advance early PD diagnosis and treatment. She helped researchers identify biomarkers of PD in sebum—the oily substance secreted by sebaceous glands.2,3 These unique chemical patterns produced as waste products of abnormal metabolism—known as volatile organic compounds (VOCs)—create the scent of illness.
As a caregiver, you know all about the sparks of experience, the early things that happen.
–Joy Milne
Based on these earlier studies, she teamed up with Drupad Trivedi, a biomedical researcher and lecturer in analytical and measurement science at the University of Manchester to identify different scent signatures produced long before PD neuromotor symptoms emerge.4 During this years-long prodromal stage, patients exhibit seemingly unrelated signs, including changes in body odor and skin health, diminished smell, constipation, and rapid eye movement (REM) sleep behaviour disorder (RBD).5,6 “Normally, during REM sleep our body is paralyzed to prevent acting out our dreams. But some people don't have this and suffer from violent movements while asleep. At least 70 percent will develop a neurological disorder in the future,” Trivedi said. Milne recalls her husband’s early symptoms, one of which was RBD. “I noticed this strange smell, but I didn't think about it, because he progressed into Parkinson's and the overwhelming smell was the Parkinson’s smell,” she said.

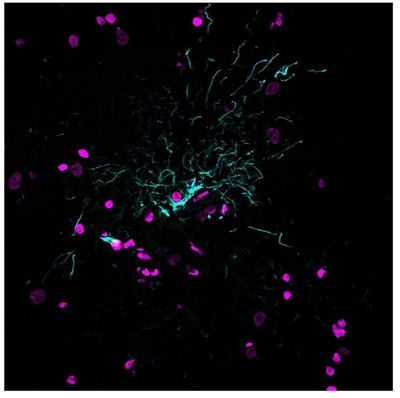
Trivedi and his team investigated whether individuals diagnosed with RBD have a unique VOC signature compared to PD patients and healthy controls, and reported their findings in a recent preprint study. They used gas chromatography, mass spectrometry, and machine learning to analyze VOCs from swab samples collected from the sebum-rich upper back area of study participants. They compared these to the scent patterns Milne identified using her own analytical instrument—an exquisitely sensitive nose. When Milne smelled the first few swabs from RBD patients she thought “Oh gosh, this is what was on the pillow!”
Trivedi and his team found that the RBD chemical signature consisted of metabolites that appear as intermediate between healthy controls and PD patients. “REM sleep disorder definitely has a different smell. It took us all by surprise” Milne said. Trivedi explained that “being able to smell something and put the pieces together was remarkable. From an analytical point of view, it means that you have a very consistent signature of volatiles that a really good nose can identify.” However, since not all individuals with RBD develop PD, additional studies are needed to determine whether the scent signature of pre-Parkinson’s RBD patients differs from that of RBD patients who do not develop PD.
See “A Nose by Any Other Name: Tracking the Scent of Tumor Metabolic Waste”
“Neurodegenerative disorders are hard to diagnose, especially early on. This study reinforces that there is a detectable change in the VOC profile in early Parkinson’s,” said Abhinav Bhushan, an assistant professor in biomedical engineering at the Illinois Institute of Technology, who was not involved in the study. “If we can diagnose early, we might be able to slow progression or treat the disease.”
Milne emphasized the essential role that caregivers play in early detection. “As a caregiver, you know all about the sparks of experience, the early things that happen. You remember the smell on the pillow, you remember having to wash and re-wash the shirts, especially around the collars, and you remember the smell changing on the head rest in the car.” Milne’s unique ability to paint her sensory world in hues of smell illuminates the past and shines an equally bright light towards future diagnosis and treatment.
References
- Milne, J. Experience: I can smell illness in people. October 21, 2022. Accessed June 2, 2023. https://www.theguardian.com/lifeandstyle/2022/oct/21/experience-i-can-smell-illnesses-in-people
- Trivedi DK, Sinclair E, Xu Y, et al. Discovery of volatile biomarkers of Parkinson's disease from sebum. ACS Cent Sci. 2019;5(4):599-606. doi:10.1021/acscentsci.8b00879
- Sinclair E, Walton-Doyle C, Sarkar D, et al. Validating differential volatilome profiles in Parkinson's disease. ACS Cent Sci. 2021;7(2):300-306. doi:10.1021/acscentsci.0c01028
- Walton-Doyle C, Heim B, Sinclair E, et al. Investigation of volatile metabolites in sebum as prodromal indicators of Parkinson’s disease. bioRxiv. Preprint posted online March 2, 2023. doi:10.1101/2023.03.01.530578
- Mantri S, Morley JF. Prodromal and early Parkinson’s disease diagnosis. May, 2018. Accessed June 2, 2023. https://practicalneurology.com/articles/2018-may/prodromal-and-early-parkinsons-disease-diagnosis
- Roguski A, Rayment D, Whone AL, et al. A Neurologist's guide to REM sleep behavior disorder. Front Neurol. 2020;11(610). doi:10.3389/fneur.2020.00610