ABOVE: (C) ISTOCK.COM, HAKAT
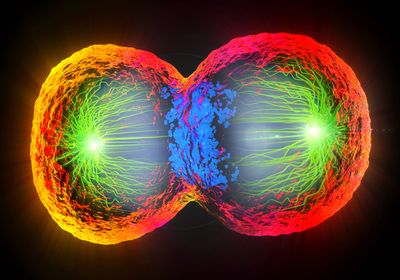
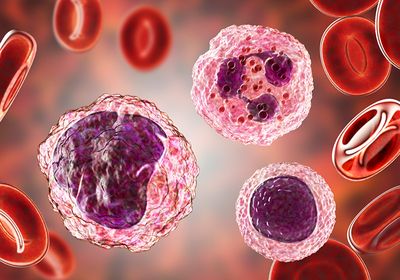
Approximately 28 million Americans have been diagnosed with heart disease.1 Traditional therapies, however, do not fully address every aspect of heart damage, and transplant organs are difficult to obtain. Human induced pluripotent stem cell-derived cardiomyocytes(iPSC-CMs) have immense potential for human disease modeling. When cultured, researchers can use patient derived iPSC-CMs to study drug efficacy and disease mechanisms. However, iPSCs begin with an embryonic phenotype, and researchers have yet to advance iPSC-CMs to a mature stage where they simulate functional heart tissue. Although scientists continue to experiment with various culture protocols, current methods are costly and time consuming.
The most exciting thing was not only seeing [the results], but then seeing other benefits that had nothing to do with what we were targeting.
- Stuart Campbell, Yale University
In a recent study published in Stem Cell Reports, Stuart Campbell and his team at Yale University presented a novel culturing method that accelerates cardiomyocyte maturation in vitro.2 “Instead of trying to explore every possible avenue, everything you could add or subtract from the media or everything that you can do to electromechanically condition the tissue, we’ve just said, let’s always look to physiology to inspire the correct conditions for inducing maturation,” said Campbell. By simultaneously applying physiological levels of calcium and delivering pulses of electric current— known as electrical pacing—to patient derived iPSCs, the researchers generated cardiomyocytes that matured in a manner that closely mimics true cardiomyocyte physiology. “Both physiological calcium and electrical pacing have been separately demonstrated in prior studies to promote cardiac maturation. However, this study unveiled an interesting and novel synergy between these two factors,” said Joseph Wu, a professor at Stanford University who was not involved in the study.
The researchers generated cardiomyocytes that showed positive force-frequency behavior—as heart tissue contraction frequencies accelerate, so does their contraction force. This phenomenon is essential for functioning heart tissue. Unexpectedly, the researchers noticed that the cells processed calcium more effectively due to an upregulation of genes involved in ion channels, sarcomeres, and fatty acid metabolism. In addition, these more mature iPSC-CMs also exhibited a robust beta-adrenergic response, an important regulator of heart function. “The most exciting thing was not only seeing [the maturation], but then seeing other benefits that had nothing to do with what we were targeting,” said Campbell. Prior to this work, Campbell mainly used computational modeling to understand cardiac disease. Therefore, crossing into the field of stem cell research presented a challenge for the lab. “It really took some persistence to get this done, and this was not something that was on my radar, or that I was particularly interested in. But this was one of those great cases where a brilliant pair of graduate students [Shi Shen and Lorenzo Sewanan] had the idea and persisted,” said Campbell. Overall, Campbell and his team presented a scalable platform that could make iPSC-CMs viable for human disease modeling, translational research, and tissue regeneration. “This study offers us a new strategy that may be combined with other existing methods such as metabolic maturation or hormone stimulation to further enhance the maturation of stem cell-derived cardiomyocytes,” said Wu.
References
- Tsao CW, et al. Heart disease and stroke statistics-2022 update: A report from the american heart association. Circulation. 2022;145(8):e153-e639.
- Shen S, et al. Physiological calcium combined with electrical pacing accelerates maturation of human engineered heart tissue. Stem Cell Reports. 2022;17(9):2037-2049.